A 24 year old man sustained a complete right-dominant hand amputation in an accident by motorcycle, in February 11, 2017 at 9:00 PM.
Cold ischemia time was 5 h at arrival. Other organ examinations were normal. He was emergently transferred to operating room where fluoroscopic study was done.
About 7 cm of the distal radius and 5 cm of the distal ulna were missing. Amputated part included proximal carpal row. Both the amputated part and proximal stump were extremely contaminated. Soft tissues were evaluated. In amputated part, there was no other injury distal-to-amputation level. Flexor and extensor tendons were cut at wrist level. Radial artery was not usable, but ulnar artery had 3 cm healthy stump. Ulnar nerve was cut 3 cm proximal to wrist and had less longitudinal damage than median nerve which was cut at about the carpal bones. Proximal stump showed much more damage. Remained ulna was 2 cm longer than radius. Some flexor and extensor muscles and tendons seemed viable, especially at the ulnar side of forearm. Median nerve had more longitudinal damage than ulnar nerve. Proximal stump of radial and ulnar arteries was damaged up to 5 m proximal to radius amputation level.
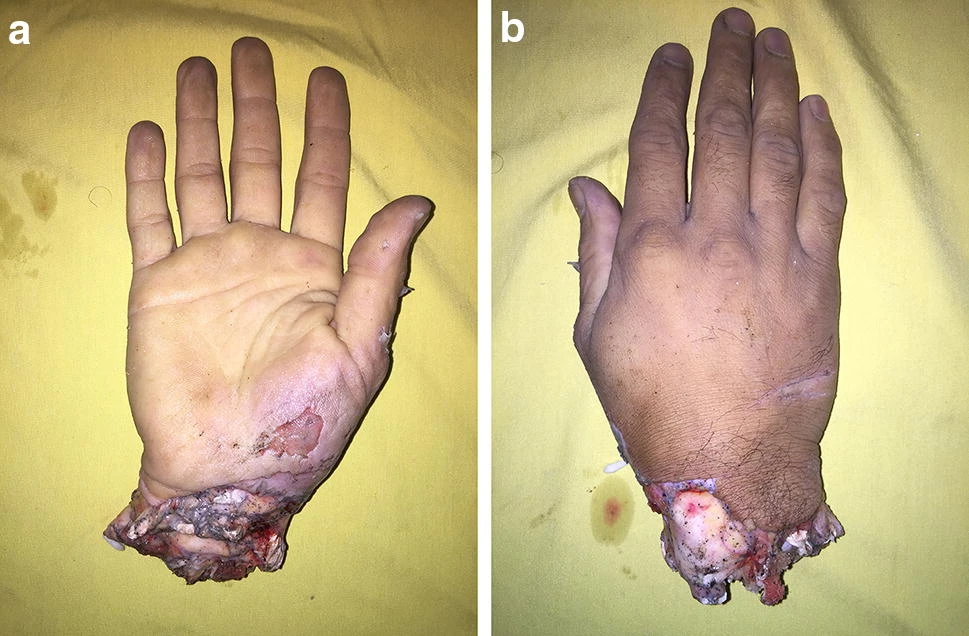
Primary replantation was not feasible because of the extent of contamination and large vascular gap. We decided to preserve the amputated part, because it was almost not injured distal-to-amputation level (Figs. 1, 2).

After complete debridement of all visible foreign bodies and crushed soft tissues of the amputated part under magnification, right leg was selected for banking (see “Discussion”). The posterior tibia artery was isolated and the saphenous vein was harvested distally. A 7 × 10 cm saphenous fasciocutaneous flap was created and elevated to provide temporary coverage. Then, end-to-end ulnar artery anastomosis was done to the posterior tibia artery. After venous blood clearance, main dorsal vein was anastomosed to saphenous vein. All other arteries and veins were ligated. Coverage was done by saphenous flap. Proximal forearm stump was then debrided under magnification. Both bones were shortened about 1 cm (Fig. 3).

Aspirin 320 mg/day, antibiotics and wound treatment, three times daily was started after operation.
Two operative sessions of debridement were performed 3 and 5 days after banking to prepare the proximal stump for final transfer (Fig. 4).

On the 8th day, banked wrist was harvested with 15 cm posterior tibia artery and 35 cm saphenous vein pedicles (Figs. 5, 6, 7, 8). Because the radius was shorter than ulna, the wrist was replanted over the ulna and fixed with two pins (Fig. 9).
Arterial anastomosis was performed 10 cm above the amputation level to the proximal ulnar artery. Venous anastomosis was performed 30 cm above the amputation level to the cephalic vein. Because only volar coverage was possible with remaining skin, saphenous vein was placed at volar aspect (Fig. 10).
The FDPS were transferred side-to-side and repaired to remnants of proximal FDP tendons. The flexor pollicis longus was repaired to the pronator teres. EDC tendons were transferred side-to-side and attached to EDC remnant muscle.
After final debridement, median nerve had 5 cm gap and ulnar nerve had extra 5 cm of healthy length. We performed nerve transposition to avoid nerve grafting. Ulnar nerve was transposed to median and median nerve was transposed to the ulnar nerve. Both nerves were rotated 180º in cooptation to cover the internal sensory–motor fascicle arrangement (Fig. 5).
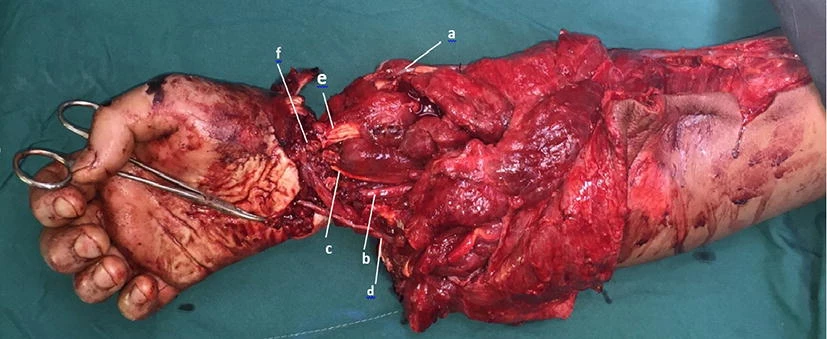
Fig 5 a Saphenous vein. b Posterior tibialis artery as the intercalary graft. c Ulnar nerve. d Median nerve. e Flexor tendons. f Flexor pollicis longus
We covered the volar side with the remaining proximal forearm skin. The saphenous flap was inset again at its original location. Minimal active motion was allowed from the postoperative day.
Six days later, exposed distal dorsal forearm was covered with a groin flap (Fig. 6).
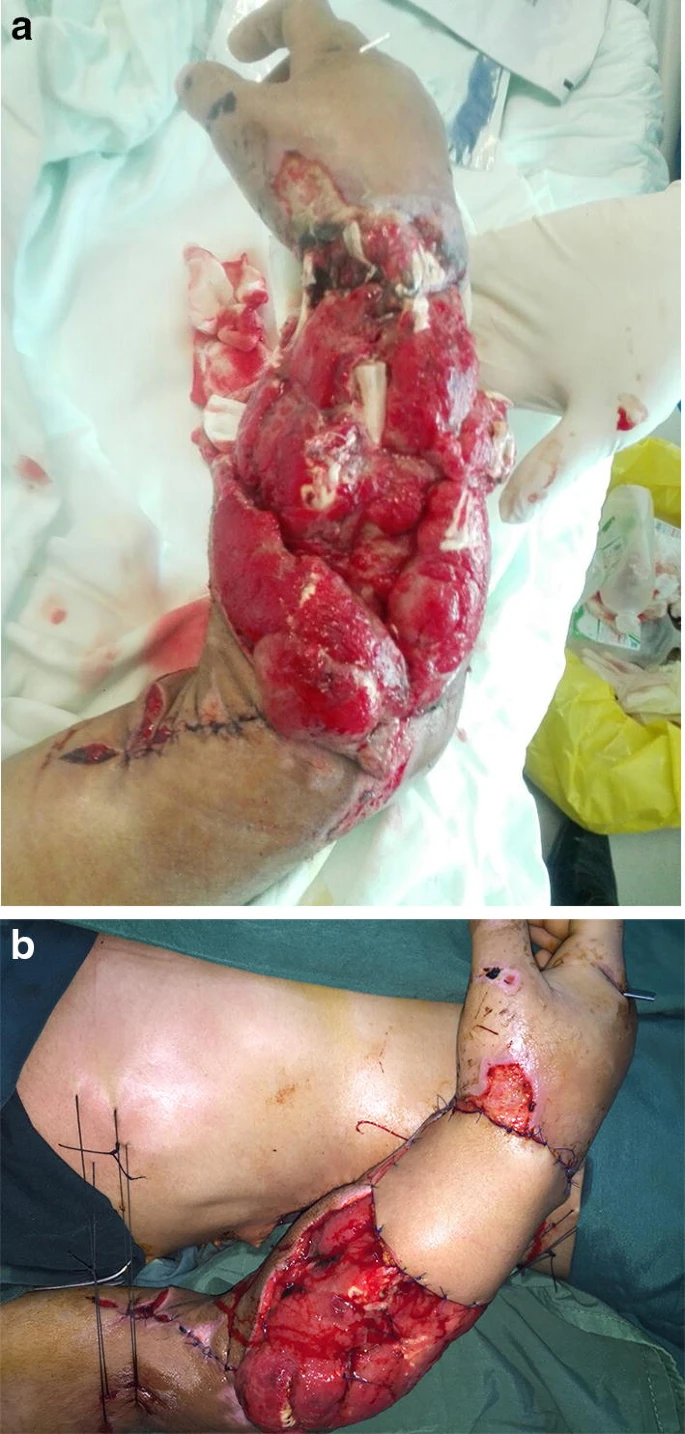
Fig 6 Wound was uncovered dorsally (a). Groin flap coverage was done for distal area with exposed radius and dorsal tendons (b)
After 2 weeks, the groin flap pedicle was incised and more proximal dorsal exposed muscle area was covered with split thickness skin graft.

Fig 7 Photography 18 months after replantation. There is 85 mm limb length discrepancy

Fig 8: Patient was assessed by qualified occupational therapist
Occupational therapy was started 2 weeks after skin grafting when all sutures were removed. Active and passive movements were improved. Eight months after replantation, pins were removed and rigid ulna-lunate fusion and bone grafting was performed (Fig. 9).

Provisional pin fixation
Fig 10 Final plate fusion
The patient was assessed 30 months after replantation; results are reflected in Table 1.
We did not encounter any complications from the anastomoses and no infection developed. The patient had no pain, weakness, or any other complaints from the donor site on the leg by the end of the follow-up.
Ectopic Banking and Implantation of an Amputated Hand Omid Liaghat1 · Zohre Shabbooie2Indian Journal of Orthopaedics (2020) 54:731–737 https://doi.org/10.1007/s43465-020-00078-7

